Amy Maxmen | (TNS) KFF Health News
A new study lends weight to fears that more livestock workers have gotten the bird flu than has been reported.
“I am very confident there are more people being infected than we know about,” said Gregory Gray, the infectious disease researcher at the University of Texas Medical Branch who led the study, posted online Wednesday and under review to be published in a leading infectious disease journal. “Largely, that’s because our surveillance has been so poor.”
As bird flu cases go underreported, health officials risk being slow to notice if the virus were to become more contagious. A large surge of infections outside of farmworker communities would trigger the government’s flu surveillance system, but by then it might be too late to contain.
“We need to figure out what we can do to stop this thing,” Gray said. “It is not just going away.”
The Centers for Disease Control and Prevention bases decisions on its surveillance. For example, the agency has bird flu vaccines on hand but has decided against offering them to farmworkers, citing a low number of cases.
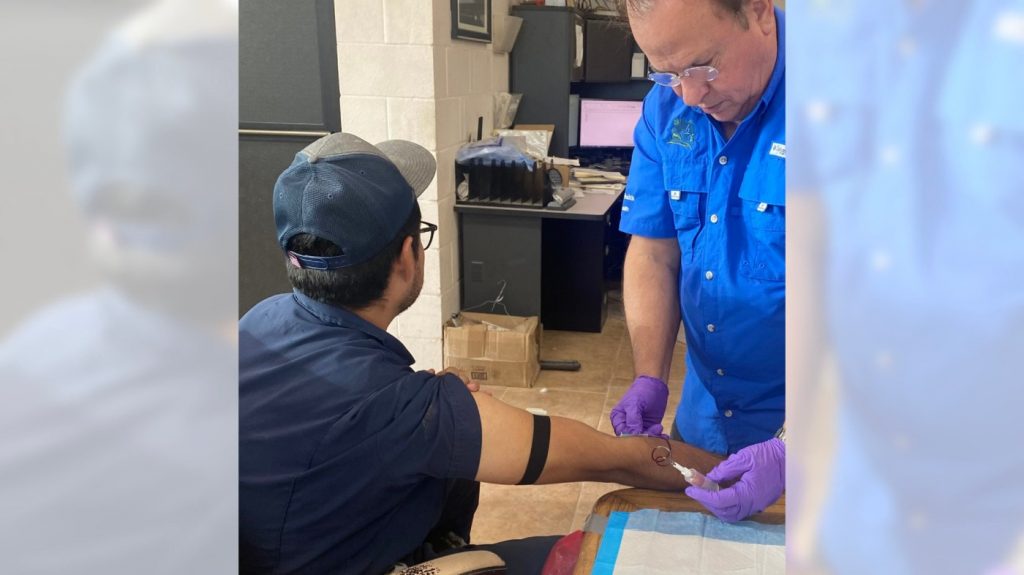
But testing for bird flu among farmworkers remains rare, which is why Gray’s research stands out as the first to look for signs of prior, undiagnosed infections in people who had been exposed to sick dairy cattle — and who had become ill and recovered.
Gray’s team detected signs of prior bird flu infections in workers from two dairy farms that had outbreaks in Texas earlier this year. They analyzed blood samples from 14 farmworkers who had not been tested for the virus and found antibodies against it in two. This is a nearly 15% hit rate from only two dairy farms out of more than 170 with bird flu outbreaks in 13 states this year.
One of the workers with antibodies had been taking medicine for a lingering cough when he agreed to allow researchers to analyze his blood in April. The other had recently recovered from a respiratory illness. She didn’t know what had caused it but told researchers that untested farmworkers around her had been sick too.
Richard Webby, director of the World Health Organization Collaborating Center for Influenza at St. Jude Children’s Research Hospital in Memphis, Tennessee, said the results confirmed his suspicions that the 13 human bird flu cases reported this year by the CDC were an undercount.
“Maybe what we see isn’t exactly the tip of the iceberg, but it’s certainly not the whole story,” Webby said.
Little testing of farmworkers
Although small, the study gives fresh urgency to reports of undiagnosed ailments among farmworkers and veterinarians. The CDC has warned that if people are infected by the seasonal flu and the bird flu simultaneously, the two types of viruses could swap genes in a way that allows the bird flu to spread between people as easily as seasonal varieties.
No evidence suggests that’s happening now. And asymptomatic cases of the bird flu appear to be rare, according to a Michigan antibody study described by the CDC on July 19. Researchers analyzed blood samples from 35 workers from dairy farms that had outbreaks in Michigan, and none showed signs of missed infections. Unlike the study in Texas, these workers hadn’t fallen sick.
“It’s a small study, but a first step,” said Natasha Bagdasarian, Michigan’s chief medical executive. She said that the state was boosting outreach to test farmworkers but its efforts were complicated by systemic issues like precarious employment that renders them vulnerable to getting fired for calling out sick.
Without more assistance for farmworkers, and cooperation between the government and the livestock industry, Gray said, the U.S. risks remaining in the dark about this virus.
“There’s a lot of genomic studies and laboratory work, but farms are where the real action is,” Gray said, “and we’re not watching.”
Communication breakdown
A dairy worker in Colorado told KFF Health News that he sought medical care about a month ago for eye irritation — a common symptom of the bird flu. The doctor conducted a usual checkup, complete with a urine analysis. But the farmworker hadn’t heard of the bird flu, and the clinician didn’t mention it or test for the virus. “They told me I had nothing,” he said in Spanish, speaking on the condition of anonymity because he feared retaliation from employers.
This dairy worker and two in Texas said their employers have not provided goggles, N95 masks, or aprons to protect them from milk and other fluids that could be contaminated with the virus. Buying their own gear is a tall order because money is tight.
As is going to the doctor. One worker in Texas said he didn’t seek care for piercing headaches and a sore throat because he doesn’t have health insurance and can’t afford the cost. He guessed the symptoms were from laboring long hours in sweltering barns with limited water. “They don’t give you water or anything,” he said. “You bring your own bottles.” But there’s no way to know the cause of symptoms — whether bird flu or something else — without testing.
About a fifth of workers on livestock farms are uninsured, according to a KFF analysis, and a similar share have household incomes of less than $40,000 a year.
The three farmworkers hadn’t heard of the bird flu from their employers or state health officials, never mind offers of tests. The CDC boasted in a recent update that, through its partnership with Meta, the company that owns Facebook and Instagram, bird flu posts have flickered across computer and smartphone screens more than 10 million times.
Such outreach is lost on farmworkers who aren’t scrolling, don’t speak English or Spanish, or are without smartphones and internet access, said Bethany Boggess Alcauter, director of research and public health programs at the National Center for Farmworker Health. She and others said that offers of protective gear from health officials weren’t reaching farms.
“We’ve heard that employers have been reticent to take them up on the offer,” said Christine Sauvé, policy and engagement manager at the Michigan Immigrant Rights Center. “If this starts to transmit more easily person to person, we’re in trouble,” she said, “because farmworker housing units are so crowded and have poor ventilation.”
Clinics might alert health officials if sick farmworkers seek medical care. But many farmworkers don’t because they lack health insurance and could be fired for missing work.
“The biggest fear we hear about is retaliation from employers, or that someone might be blacklisted from other jobs,” Sauvé said.
Flu surveillance
The CDC assesses the current bird flu situation as a low public health risk because the country’s flu surveillance system hasn’t flagged troubling alerts.
The system scans for abnormal increases in hospital visits. Nothing odd has turned up there. It also analyzes a subset of patient samples for unusual types of flu viruses. Since late February, the agency has assessed about 36,000 samples. No bird flu.
However, Samuel Scarpino, an epidemiologist who specializes in disease surveillance, said this system would miss many emerging health threats because, by definition, they start with a relatively small number of infections. Roughly 200,000 people work on farms with livestock in the United States, according to the CDC. That’s a mere 0.1% of the country’s population.
Scarpino said the CDC’s surveillance would be triggered if people started dying from the bird flu. The 13 known cases have been mild. And the system will probably pick up surges if the virus spreads beyond farmworkers and their closest contacts — but by then it may be too late to contain.
“We don’t want to find ourselves in another covid situation,” Scarpino said, recalling how schools, restaurants, and businesses needed to close because the coronavirus was too widespread to control through testing and targeted, individual isolation. “By the time we were catching cases,” he said, “there were so many that we were only left with bad options.”
Troubling signs
Researchers warn that the H5N1 bird flu virus has evolved to be more infectious to mammals, including humans, in the past couple of years. This drives home the need to keep an eye on what’s happening as the outbreak spreads to dairy farms across the country.
The bird flu virus appears be spreading mainly through milk and milking equipment. But for the first time, researchers reported in May and July that it spread inefficiently through the air between a few laboratory ferrets kept inches apart. And in cattle experiments, some cows were infected by breathing in virus-laden microscopic droplets — the sort of thing that could happen if an infected cow was coughing in close proximity to another.
Cows do, in fact, cough. The new study from Texas notes that cattle coughed during outbreaks on the farms and showed other signs of respiratory illness.
Other observations were ominous: About half of some 40 cats on one farm died suddenly at the peak of its outbreak, probably from lapping up raw milk suffused with bird flu virus.
Most people diagnosed with the bird flu have been infected from animals. In his new study, Gray saw a hint that the virus may occasionally spread from person to person, but he added that this remains conjecture. One of the two people who had antibodies worked in the farm’s cafeteria adjacent to the milking parlor — alongside farmworkers but not cattle.
“We need to find ways to have better surveillance,” he said, “so we can make informed decisions rather than decisions based on guesswork.”
(KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs of KFF — the independent source for health policy research, polling and journalism.)
©2024 KFF Health News. Distributed by Tribune Content Agency, LLC.